 Alopecia
areata (AA) is probably the third most common
form of hair loss dermatologists see, after
androgenetic alopecia and telogen effluvium.
The lifetime risk for AA is nearly 2%, or two
in every 100 people will get AA at some point
in their lives. It is not contagious; you can't
catch AA from someone who has it. Alopecia
areata (AA) is probably the third most common
form of hair loss dermatologists see, after
androgenetic alopecia and telogen effluvium.
The lifetime risk for AA is nearly 2%, or two
in every 100 people will get AA at some point
in their lives. It is not contagious; you can't
catch AA from someone who has it.
Researchers believe AA is an autoimmune disease
such as rheumatoid arthritis, but in this case
the individual's own immune system attacks hair
follicles instead of bone joints. Just why or
how AA develops is not clear. For whatever reason,
the immune system is inappropriately activated
and attacks hair follicles. Research using several
disease models shows certain types of lymphocytes
play a primary role in the hair loss. They seem
to attack the hair follicles, mistakenly thinking
that somehow they are a threat to the rest of
the body.
AA can affect men, women, and children. It often
appears as well-defined circular bald patches
on the scalp. Many people will get just one
or two patches, but for some the hair loss can
be extensive. Unfortunately, children who develop
AA before puberty are most likely to develop
more extensive and persistent hair loss.
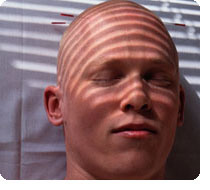
Hair loss that spreads to cover the entire scalp
is called alopecia totalis. If it spreads over
the entire body, affecting scalp, eyebrows,
lashes, beard, pubic hair, and everything else,
then the condition is called alopecia universalis.
If the alopecia is just limited to the beard
area in men, it is called alopecia barbae.
The inflammation involved in AA focuses on the
roots of hair follicles deep in the skin. As
a result there is very little visible at the
skin surface. There is no redness and often
no pain, although a few people do find their
skin itchy or painful to touch in the very early
stages of AA development. Usually, though, there
is no sensation -- just a patchy shedding of
hair.
The hair loss can be quite sudden, developing
in a matter of a few days and it may happen
anywhere on the scalp. The patch is usually
smooth bald skin with nothing obvious to see
beyond the absence of hair. Unlike other autoimmune
diseases, the target of the inflammatory response
in AA, the hair follicles, are not completely
destroyed and can re-grow if the inflammation
subsides.
People with just one or two patches of AA often
have a full and spontaneous recovery within
two years whether or not they receive treatment.
However, about 30% of individuals find the condition
persists and becomes more extensive, or they
have repeated cycles of hair loss and re-growth.
Traditionally, AA has been regarded as a stress-induced
disease. Unfortunately that view persists today,
even among some dermatologists, even though
very little scientific evidence supports the
view.
AA is much more complicated. Extreme stress
might trigger AA in some people, but recent
research shows that genes can also be involved.
There are probably several genes that can make
an individual more susceptible to developing
AA. The more of these genes a person has, the
more likely they will develop AA.
Some researchers believe there are a wide range
of contributing factors that make someone more
susceptible to developing AA. Hormones, allergies,
viruses, and even toxins might contribute. Probably
several factors combined are involved in the
activation of AA in any one individual.
Treatments for Alopecia
There are a range of treatments for AA, but
none are effective for everyone and some people
with AA don't respond to any treatment. Because
some of the available treatments have a high
risk of side effects, they are often not used
for children.
The most common AA treatment involves the use
of corticosteroids. Corticosteroid creams applied
to the bald patches are popular with the average
dermatologist, although this treatment approach
is only successful for the very mildest cases.
A more potent approach is to inject corticosteroid
solutions into the bald patches. This can work
well for some people, but close monitoring is
required to ensure that side effects, such as
skin thinning at the site of injection, do not
occur.
In extensive cases, systemic corticosteroids
(those taken in pill or other form to affect
your body) are used, though not continuously
since they can cause significant side effects
like bone thinning. But short-term "pulse
therapy" often has good results.
More specialized treatment approaches involve
the application of contact sensitizing chemicals
to the skin. These cause an allergic reaction
that can help promote hair growth. That may
sound counterintuitive but it seems to work.
A variety of experimental approaches are currently
in laboratory and clinical trials. One group
of drugs being tested are "biologics,"
which have bits of protein that interfere in
a very specific way with the activity of immune
cells. Biologics are injected systemically to
damp down the immune activity and allow hair
to regrow. The results of these trials are awaited
with much interest.
Unfortunately, people with more extensive, long-term
AA find the treatments currently available do
not work well. For these individuals the only
practical answer is a wig and lots of emotional
support. It can be depressing not to have hair,
especially for children, who don't want to be
different from their classmates at school, and
women. In North America and many other countries
of the world, you can access a network of support
agencies for people with AA. Details are on
the National Alopecia Areata Foundation website
(http://www.naaf.org).
 |
|
 |
|
